Long-term COVID-19 complications, often referred to as “long COVID” or “post-acute sequelae of SARS-CoV-2 infection (PASC),” have emerged as a significant public health concern. This condition encompasses a wide range of persistent symptoms and health problems that some individuals experience after recovering from the acute phase of COVID-19. Understanding the scope, mechanisms, and management strategies of long-term COVID-19 complications is crucial for healthcare providers, patients, and policymakers.
Introduction
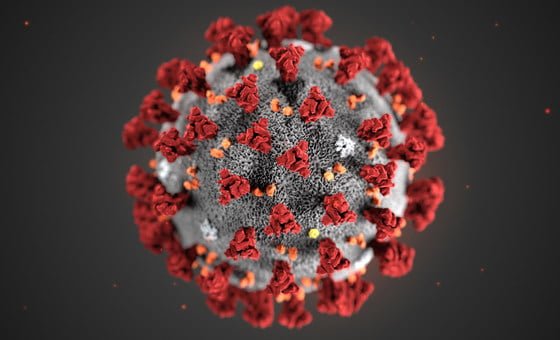
COVID-19, caused by the SARS-CoV-2 virus, was initially identified as a respiratory illness. However, it has since been recognized to affect multiple organ systems, leading to a broad spectrum of symptoms and complications. While most individuals recover completely, a subset experiences lingering or new symptoms that can last weeks, months, or potentially years after the initial infection, defining long COVID.
Epidemiology
The prevalence of long COVID varies widely across studies, with estimates suggesting that approximately 10-30% of individuals who contract COVID-19 will experience some form of long-term symptoms. These rates are influenced by factors such as the severity of the initial illness, age, sex, and the presence of pre-existing health conditions.
Clinical Manifestations
Long COVID can present with a diverse array of symptoms affecting different body systems, including but not limited to:
- Respiratory symptoms: Persistent cough, difficulty breathing, and chest pain.
- Neurological symptoms: Brain fog, headaches, sleep disturbances, dizziness, and neuropathy.
- Cardiovascular symptoms: Palpitations, chest pain, and increased risk of heart failure or thrombosis.
- Gastrointestinal symptoms: Abdominal pain, diarrhea, and nausea.
- Musculoskeletal symptoms: Joint pain and muscle aches.
- Psychological/psychiatric symptoms: Depression, anxiety, and mood swings.
Pathophysiology
The exact mechanisms underlying long COVID are not fully understood, but several hypotheses have been proposed, including:
- Persistent viral reservoirs leading to ongoing immune activation.
- Autoimmune responses triggered by the virus.
- Organ damage incurred during the acute phase of the infection.
- Microvascular injury leading to impaired blood flow and tissue oxygenation.
Diagnosis
Diagnosing long COVID is challenging due to the heterogeneity of symptoms and the lack of specific diagnostic criteria. A comprehensive history and physical examination, alongside a multidisciplinary approach involving various specialists, are often required. Laboratory and imaging studies are tailored to the presenting symptoms to rule out alternative diagnoses.
Management and Treatment
Management of long COVID is primarily symptomatic and multidisciplinary, aiming to improve quality of life and function. Treatment strategies may include:
- Rehabilitation services (physical, occupational, and speech therapy)
- Pharmacological interventions for specific symptoms (e.g., pain management, sleep aids)
- Psychological support for mental health symptoms
- Lifestyle modifications (e.g., graded exercise therapy, nutritional support)
Prevention and Public Health Implications
Preventing COVID-19 infection through vaccination and public health measures is the most effective strategy to reduce the risk of long COVID. Public health campaigns and policies should continue to emphasize the importance of vaccination, mask-wearing, and social distancing to control the spread of the virus.
Conclusion
Long-term COVID-19 complications represent a complex and evolving challenge with significant implications for individuals and healthcare systems worldwide. Ongoing research is crucial to unravel the pathophysiological mechanisms, develop diagnostic criteria, and identify effective treatments. Multidisciplinary care, patient education, and support are key components in managing the diverse manifestations of long COVID. As our understanding of this condition evolves, so too will our strategies for prevention, diagnosis, and management, ultimately improving outcomes for those affected.